Complex PTSD develops in response to chronic traumatisation over the course of months or years. The trauma can include emotional, physical or sexual abuse. There are exceptional circumstances in which adults can develop Complex PTSD, but it is mostly seen in those whose trauma occurred in childhood. When children go through prolonged trauma the brain is still developing and it interrupts the natural course of their psychological and neurological development.
Psychological effects of Complex PTSD include hypervigilance, this is where the person is always on high alert both mentally and physically as they are constantly on the lookout for danger. They may have a hyper awareness of sounds, facial expressions or the atmosphere in a room. They may have an exaggerated startle response, or they may be ‘triggered’ by people arguing or shouting. This means that the nervous system is triggered into producing all the chemicals necessary and getting the body ready for the fight, flight, freeze or submit response. Complex PTSD means the person can feel easily overwhelmed and less resilient to life’s issues. They may worry extensively about what may happen, they may have nightmares and flashbacks to the trauma, and they may feel depressed or hopeless about the future. They can also be irritable and quick to anger and may have problems sleeping.
Individuals with Complex PTSD are also vulnerable to physical symptoms that cannot be explained medically but are caused by their internal pain and stress. These somatic symptoms can include neck and back pain, headaches and migraines, gastrointestinal problems including irritable bowel syndrome. They may develop fibromyalgia which involves muscle pain, fatigue, and problems with sleep, memory, and mood.
Complex PTSD very often co-occurs with dissociative disorders. Other common conditions it co-occurs with include borderline personality disorder, depressive or bipolar disorders, anxiety disorders, obsessive compulsive disorders, eating disorders and addictions.
Judith Herman is a psychiatrist who studied trauma extensively. She developed the three stages of trauma recovery below:
Stage One: Safety and Stabilisation – Overcoming dysregulation
The aim of this stage of therapy is for the client to learn to calm their nervous system and to feel safer in the here and now (rather than continually reliving the trauma).
- setting goals with the counsellor regarding what the client would like to work on
- improving the sense of personal stability and safety
- using techniques to develop self-awareness
- practicing self-care
- developing self-compassion
- developing resilience
- learning to identify and manage triggers
Read about different triggers and how they feel here.
Stage Two: Coming to Terms with the Traumatic Memories
Clients from backgrounds of trauma can be phobic of their feelings and memories. There can be repressed feelings and memories. At stage two the client works to overcome any fear they have of traumatic memories so that they can be integrated.
- working through painful and traumatic memories
- mourning any losses associated with the trauma
- permitting the self to grieve
- mourning the loss of good experiences or opportunities due to trauma
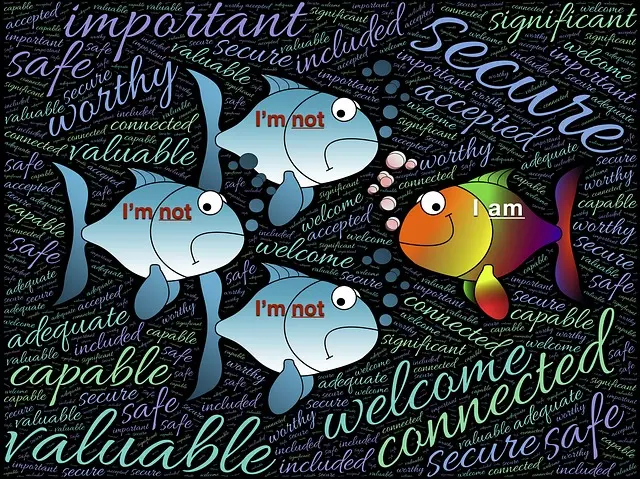
Stage Three: Integration
By stage three, the client has a good understanding of themselves and their past which no longer has so much influence over their behaviour. Much of the unconscious has been made conscious and they can manage their emotions well. They can work on overcoming any fears they may have of normal life and start to construct a healthy, fulfilling existence. A lot of healing has been done by this stage and many Complex PTSD symptoms will have resolved themselves. Feelings of shame and alienation will have decreased.